Soap Note Template

Introduction to Soap Note Template

A SOAP note is a method of documentation used by healthcare professionals to record patient information in a clear and concise manner. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which are the four main components of the note. In this article, we will delve into the details of a SOAP note template, its importance, and how it is used in clinical practice.
Key Points
- The SOAP note template is a widely used method of documentation in healthcare settings.
- It consists of four main components: Subjective, Objective, Assessment, and Plan.
- Each component serves a unique purpose in patient care and documentation.
- The SOAP note template helps healthcare professionals to communicate effectively and provide high-quality patient care.
- It is an essential tool for healthcare providers to document patient information, track progress, and make informed decisions.
Components of a SOAP Note Template
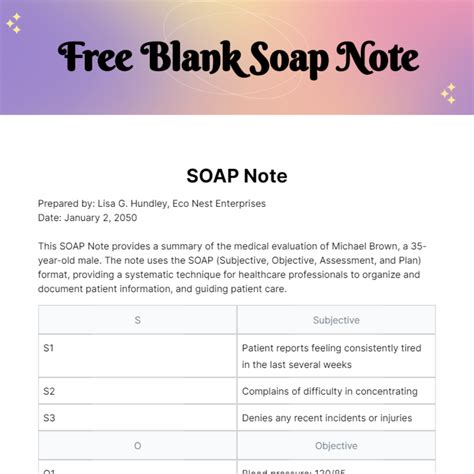
A SOAP note template typically consists of four main components: Subjective, Objective, Assessment, and Plan. Each component is designed to capture specific information about the patient’s condition, treatment, and progress.
Subjective Component
The subjective component of the SOAP note template includes information provided by the patient, such as their symptoms, medical history, and concerns. This information is essential in understanding the patient’s perspective and developing an effective treatment plan.
Objective Component
The objective component of the SOAP note template includes information that can be measured or observed, such as vital signs, laboratory results, and physical examination findings. This information helps healthcare professionals to assess the patient’s condition and track their progress over time.
Assessment Component
The assessment component of the SOAP note template involves the healthcare professional’s interpretation of the subjective and objective data. This component includes the diagnosis, prognosis, and any relevant medical conditions or concerns.
Plan Component
The plan component of the SOAP note template outlines the treatment plan, including any medications, therapies, or interventions that will be used to manage the patient’s condition. This component also includes any follow-up appointments, tests, or procedures that are necessary.
| Component | Description |
|---|---|
| Subjective | Patient-provided information, such as symptoms and medical history |
| Objective | Measurable or observable information, such as vital signs and laboratory results |
| Assessment | Healthcare professional's interpretation of subjective and objective data |
| Plan | Treatment plan, including medications, therapies, and follow-up appointments |
Importance of SOAP Note Template in Clinical Practice
The SOAP note template is widely used in clinical practice due to its ability to facilitate effective communication and high-quality patient care. By using this template, healthcare professionals can ensure that patient information is accurately documented and easily accessible.
Benefits of SOAP Note Template
The SOAP note template offers several benefits, including improved communication, increased efficiency, and enhanced patient care. By using this template, healthcare professionals can reduce errors, improve patient outcomes, and enhance the overall quality of care.
Challenges and Limitations of SOAP Note Template
Despite its benefits, the SOAP note template also has some challenges and limitations. One of the main limitations is the potential for incomplete or inaccurate information, which can lead to errors in patient care. Additionally, the template may not be suitable for all clinical settings or patient populations.
What is the purpose of a SOAP note template?
+The purpose of a SOAP note template is to provide a standardized method of documentation that facilitates effective communication and high-quality patient care.
What are the components of a SOAP note template?
+The components of a SOAP note template include subjective, objective, assessment, and plan.
Why is the SOAP note template important in clinical practice?
+The SOAP note template is important in clinical practice because it facilitates effective communication, increases efficiency, and enhances patient care.
In conclusion, the SOAP note template is a valuable tool for healthcare professionals to communicate effectively and provide high-quality patient care. By understanding the components and importance of this template, healthcare providers can ensure that patient information is accurately documented and easily accessible, leading to improved patient outcomes and enhanced quality of care.